A 35 years old male patient with hepatic encephalopathy
This is online elog book to discuss for patients deidentified health data shared after taking her/guardians signed informed consent
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.
A 35 years old male patient present to the opd with chief complains of altered sensorium,yellow discoloration of sclera, pedal edema since 1 week.
History of present illness
Patient was apparently asymptomatic 6 years back. Then he developed yellowish discoloration of sclera in 2014 with altered sensorium so he took treatment in hospital in Hyderabad.
Where he was diagnosed as the chronic liver disease. From then he was on medication.
Patient has habit of alcohol, so he was adviced not to consume alcohol.
He stopped the medication and continued drinking alcohol.
He had fever from 4 days which is subsided on medication.
History of loose stools since 4 days.
History of altered Sensorium.
History of malena, pain abdomen.
Past history
No history of diabetes, hypertension, asthma, epilepsy.
History of tuberculosis 15 years back.
Personal history
Mixed diet
Irregular bowel and bladder movements.
Loss of appetite.
Sleep adequate.
Patient had habit of consuming alcohol since 20 years. Consumes regular 90ml thrice in a day.
Treatment history
He took medication for liver disease 6 years back and stopped.
Not allergic to any known drugs.
General examination
Patient is unconscious, no response to the commands.
Poor body built and malnourished.
Jaundice is present
Pedal edema is present
No pallor
No clubbing
No cyanosis
No generalised lymphadenopathy
Vitals :
Temp : Afebrile
BP : 80/60 mm Hg
PR : 105 bpm
RR : 25 cpm
GRBS : 33 mg / dl
SpO2 : 91 % @ RA
Systemic Examination :
Cardiovascular system
Chest wall is bilaterally symmetrical.
No pericadial bulge.
No visible pulsations.
S1, S2 heard. No murmurs.
Respiratory system:
BAE +
Crepts present.
Per abdomen:
Distended abdomen
Central nervous system:
Patient is unconscious.
No response to commands.
INVESTIGATIONS:
ECG:
On 14/12/2021
On 16/12/2021:









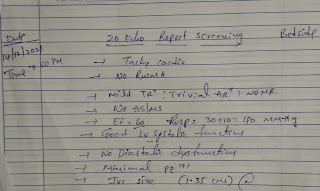






Comments
Post a Comment