Final exam long case
This is online elog book to discuss for patients deidentified health data shared after taking her/guardians signed informed consent
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.
A 18 years old female patient presented to the opd with chief complaint of fever since 3months, joint pains since 2 months, vomitings 2months back for 1 week, headache 2months back.
History of present illness
Patient was apparently asymptomatic 3months back then she developed fever, after the fever subsided she developed pain at the interphalangeal joints of left hand. Then later to the other joints of hands and legs which relieved on medication and relapse after stopping the medication
She had history of fever along with multiple joint pains. (small joints of hand ----> elbow---->shoulder joint).
Patient had a h/O migratory polyarthritis.
H/O dragging type of pain in both lower limbs.
H/O decreases appetite since 2months.h/o abdominal pain since 5days back. H/O vomitings since 2-3 days, non-bilious, non-projectile containing food particles.
H/O of headache,burning sensation in the eyes.
Past history
Not a known case of diabetes mellitus, hypertension, asthma, thyroid, TB.
No history of any major surgeries in the past.
Personal history
Appetite- decreased since 2months.
Diet - mixed
Regular bowel and bladder movements.
Sleep adequate
Menstrual history
Menarche at the age of 13 years.
Regular menstrual cycle.
General examination
Patient is concious, coherent and co-operative. Well oriented to the time, place and person.
Well nourished and moderate built.
Pallor is present.
No icterus, cyanosis, clubbing, generalised lymphadenopathy, pedal edema.
Vitals
Temp: afebrile
Pulse rate: 83 bpm
Respiratory rate:18 cycles/min
Blood pressure: 110/60 mmhg.
Spo2: 98%
GRBS: 120mg/ dl
Systemic examination
CVS:
S1, S2 heard
No murmurs heard.
Respiratory system
Bilateral airway +
NVBS +
Per abdomen:
Soft, non tender
CNS:
Concious
No abnormality detected.
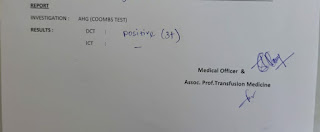
Investigations:
ECG:
X- ray:
Ultra sound report:
FEVER WITH POLYARTHRITIS (SECONDARY TO RA? OR SLE?) UNDER EVALUATION
TREATMENT;-
1)T. ULTRACET (325MG+37.5MG) PO/QID
2)T.ZOFER (MD) 4MG PO/SOS
3)T.ZINCOVIT PO/BD
4)T.LIMCEE PO/BD
5)T.PAN 40 MG PO/OD.
















Comments
Post a Comment